CANCER
Cancer is a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body
Understanding cancer at cellular level
Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body needs them. When cells grow old or become damaged, they die, and new cells take their place.
Sometimes this orderly process breaks down, and abnormal or damaged cells grow and multiply when they shouldn’t. These cells may form tumors, which are lumps of tissue. Tumors can be cancerous or not cancerous (benign).
01
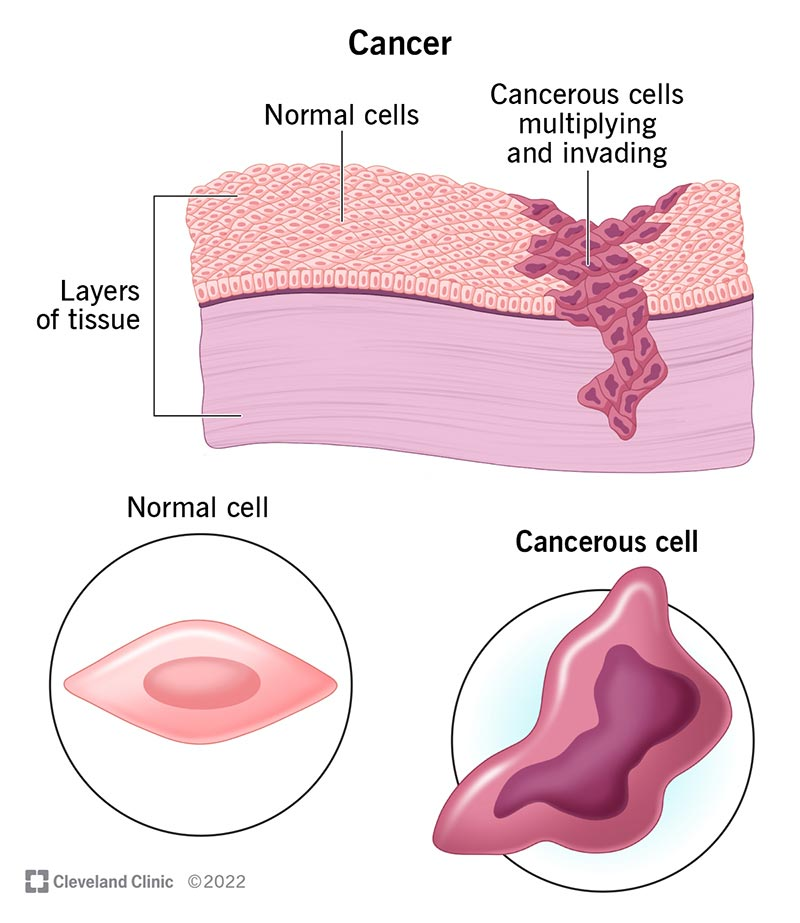
Cancer happens when normal cells become cancerous cells that multiply and spread.
02
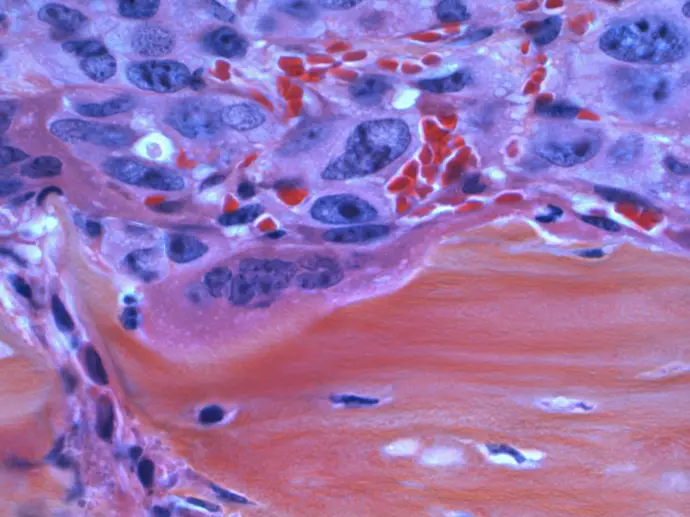
A dividing breast cancer cell.
03
Cancerous cells is an abnormal cell that grows and divides uncontrollably whereas normal cells is a healthy cell that grows, divides, and dies in a controlled and organized way.
04
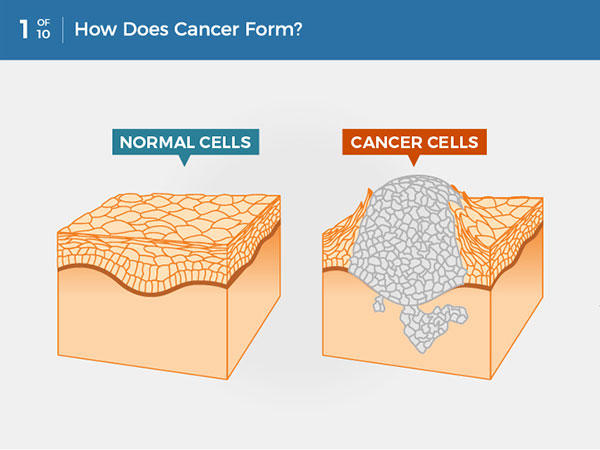
Cancer is a disease caused when cells divide uncontrollably and spread into surrounding tissues.
Tumours-An overview
Cancerous tumors spread into, or invade, nearby tissues and can travel to distant places in the body to form new tumors (a process called metastasis). Cancerous tumors may also be called malignant tumors. Many cancers form solid tumors, but cancers of the blood, such as leukemias, generally do not.
Benign tumors do not spread into, or invade, nearby tissues. When removed, benign tumors usually don’t grow back, whereas cancerous tumors sometimes do. Benign tumors can sometimes be quite large, however. Some can cause serious symptoms or be life threatening, such as benign tumors in the brain.
Cancerous cells and Normal cells differences-
Cancer cells differ from normal cells in many ways. For instance, cancer cells:
- grow in the absence of signals telling them to grow. Normal cells only grow when they receive such signals.
- ignore signals that normally tell cells to stop dividing or to die (a process known as programmed cell death, or apoptosis).
- invade into nearby areas and spread to other areas of the body. Normal cells stop growing when they encounter other cells, and most normal cells do not move around the body.
- tell blood vessels to grow toward tumors. These blood vessels supply tumors with oxygen and nutrients and remove waste products from tumors.
- hide from the immune system. The immune system normally eliminates damaged or abnormal cells.
- trick the immune system into helping cancer cells stay alive and grow. For instance, some cancer cells convince immune cells to protect the tumor instead of attacking it.
- accumulate multiple changes in their chromosomes, such as duplications and deletions of chromosome parts. Some cancer cells have double the normal number of chromosomes.
- rely on different kinds of nutrients than normal cells. In addition, some cancer cells make energy from nutrients in a different way than most normal cells. This lets cancer cells grow more quickly.
Many times, cancer cells rely so heavily on these abnormal behaviors that they can’t survive without them. Researchers have taken advantage of this fact, developing therapies that target the abnormal features of cancer cells. For example, some cancer therapies prevent blood vessels from growing toward tumors, essentially starving the tumor of needed nutrients.
How does Cancer develop?
Cancer is caused by certain changes to genes, the basic physical units of inheritance. Genes are arranged in long strands of tightly packed DNA called chromosomes.
Genetic changes that cause cancer can happen because:
- of errors that occur as cells divide.
- of damage to DNA caused by harmful substances in the environment, such as the chemicals in tobacco smoke and ultraviolet rays from the sun. (Our Cancer Causes and Prevention section has more information.)
- they were inherited from our parents.
The body normally eliminates cells with damaged DNA before they turn cancerous. But the body’s ability to do so goes down as we age. This is part of the reason why there is a higher risk of cancer later in life.
Each person’s cancer has a unique combination of genetic changes. As the cancer continues to grow, additional changes will occur. Even within the same tumor, different cells may have different genetic changes.

Cancer is caused by certain changes to genes, the basic physical units of inheritance. Genes are arranged in long strands of tightly packed DNA called chromosomes.
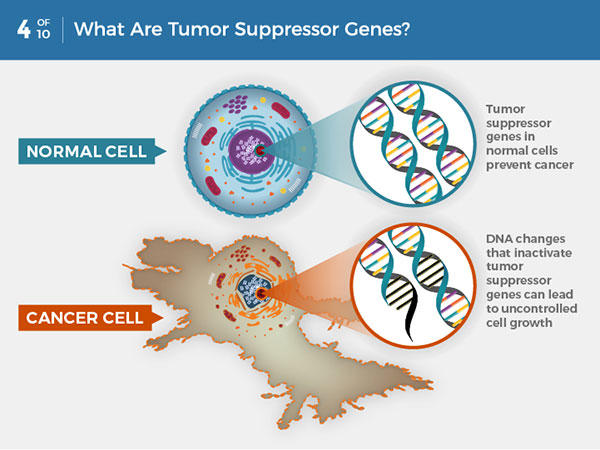
A DNA change can cause genes involved in normal cell growth to become oncogenes. Unlike normal genes, Oncogenes cannot be turned off ,so they cause uncontrolled cell growth
Growth
Cancer Cells
When Cancer spreads
A cancer that has spread from the place where it first formed to another place in the body is called metastatic cancer. The process by which cancer cells spread to other parts of the body is called metastasis.
Metastatic cancer has the same name and the same type of cancer cells as the original, or primary, cancer. For example, breast cancer that forms a metastatic tumor in the lung is metastatic breast cancer, not lung cancer.
Under a microscope, metastatic cancer cells generally look the same as cells of the original cancer. Moreover, metastatic cancer cells and cells of the original cancer usually have some molecular features in common, such as the presence of specific chromosome changes.
In some cases, treatment may help prolong the lives of people with metastatic cancer. In other cases, the primary goal of treatment for metastatic cancer is to control the growth of the cancer or to relieve symptoms it is causing. Metastatic tumors can cause severe damage to how the body functions, and most people who die of cancer die of metastatic disease.
Types of Genes that Cause Cancer
The genetic changes that contribute to cancer tend to affect three main types of genes—proto-oncogenes, tumor suppressor genes, and DNA repair genes. These changes are sometimes called “drivers” of cancer.
Proto-oncogenes are involved in normal cell growth and division. However, when these genes are altered in certain ways or are more active than normal, they may become cancer-causing genes (or oncogenes), allowing cells to grow and survive when they should not.
Tumor suppressor genes are also involved in controlling cell growth and division. Cells with certain alterations in tumor suppressor genes may divide in an uncontrolled manner.
DNA repair genes are involved in fixing damaged DNA. Cells with mutations in these genes tend to develop additional mutations in other genes and changes in their chromosomes, such as duplications and deletions of chromosome parts. Together, these mutations may cause the cells to become cancerous.
As scientists have learned more about the molecular changes that lead to cancer, they have found that certain mutations commonly occur in many types of cancer. Now there are many cancer treatments available that target gene mutations found in cancer. A few of these treatments can be used by anyone with a cancer that has the targeted mutation, no matter where the cancer started growing.
Tissue Changes that Are Not Cancer
Not every change in the body’s tissues is cancer. Some tissue changes may develop into cancer if they are not treated, however. Here are some examples of tissue changes that are not cancer but, in some cases, are monitored because they could become cancer:
- Hyperplasia occurs when cells within a tissue multiply faster than normal and extra cells build up. However, the cells and the way the tissue is organized still look normal under a microscope. Hyperplasia can be caused by several factors or conditions, including chronic irritation.
- Dysplasia is a more advanced condition than hyperplasia. In dysplasia, there is also a buildup of extra cells. But the cells look abnormal and there are changes in how the tissue is organized. In general, the more abnormal the cells and tissue look, the greater the chance that cancer will form. Some types of dysplasia may need to be monitored or treated, but others do not. An example of dysplasia is an abnormal mole (called a dysplastic nevus) that forms on the skin. A dysplastic nevus can turn into melanoma, although most do not.
- Carcinoma in situ is an even more advanced condition. Although it is sometimes called stage 0 cancer, it is not cancer because the abnormal cells do not invade nearby tissue the way that cancer cells do. But because some carcinomas in situ may become cancer, they are usually treated.
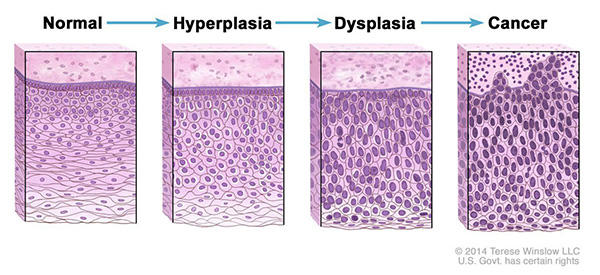
Normal cells may become cancer cells.Before cancer cells form in tissues of the body, the cells go through abnormal changes called hyperplasia and dysplasia. In hyperplasia, there is an increase in the number of cells in an organ or tissue that appear normal under a microscope. In dysplasia, the cells look abnormal under a microscope but are not cancer. Hyperplasia and dysplasia may or may not become cancer.
Types of Cancer
There are more than 100 types of cancer. Types of cancer are usually named for the organs or tissues where the cancers form. For example, lung cancer starts in the lung, and brain cancer starts in the brain. Cancers also may be described by the type of cell that formed them, such as an epithelial cell or a squamous cell.
Cancers that begin in specific types of cells
Carcinoma
Carcinomas are the most common type of cancer. They are formed by epithelial cells, which are the cells that cover the inside and outside surfaces of the body. There are many types of epithelial cells, which often have a column-like shape when viewed under a microscope.
Carcinomas that begin in different epithelial cell types have specific names:
Adenocarcinoma is a cancer that forms in epithelial cells that produce fluids or mucus. Tissues with this type of epithelial cell are sometimes called glandular tissues. Most cancers of the breast, colon, and prostate are adenocarcinomas.
Basal cell carcinoma is a cancer that begins in the lower or basal (base) layer of the epidermis, which is a person’s outer layer of skin.
Squamous cell carcinoma is a cancer that forms in squamous cells, which are epithelial cells that lie just beneath the outer surface of the skin. Squamous cells also line many other organs, including the stomach, intestines, lungs, bladder, and kidneys. Squamous cells look flat, like fish scales, when viewed under a microscope. Squamous cell carcinomas are sometimes called epidermoid carcinomas.
Transitional cell carcinoma is a cancer that forms in a type of epithelial tissue called transitional epithelium, or urothelium. This tissue, which is made up of many layers of epithelial cells that can get bigger and smaller, is found in the linings of the bladder, ureters, and part of the kidneys (renal pelvis), and a few other organs. Some cancers of the bladder, ureters, and kidneys are transitional cell carcinomas.
Sarcoma
Sarcomas are cancers that form in bone and soft tissues, including muscle, fat, blood vessels, lymph vessels, and fibrous tissue (such as tendons and ligaments).
Osteosarcoma is the most common cancer of bone. The most common types of soft tissue sarcoma are leiomyosarcoma, Kaposi sarcoma, malignant fibrous histiocytoma, liposarcoma, and dermatofibrosarcoma protuberans
Leukemia
Cancers that begin in the blood-forming tissue of the bone marrow are called leukemias. These cancers do not form solid tumors. Instead, large numbers of abnormal white blood cells (leukemia cells and leukemic blast cells) build up in the blood and bone marrow, crowding out normal blood cells. The low level of normal blood cells can make it harder for the body to get oxygen to its tissues, control bleeding, or fight infections.
There are four common types of leukemia, which are grouped based on how quickly the disease gets worse (acute or chronic) and on the type of blood cell the cancer starts in (lymphoblastic or myeloid). Acute forms of leukemia grow quickly and chronic forms grow more slowly.
Lymphoma
Lymphoma is cancer that begins in lymphocytes (T cells or B cells). These are disease-fighting white blood cells that are part of the immune system. In lymphoma, abnormal lymphocytes build up in lymph nodes and lymph vessels, as well as in other organs of the body.
There are two main types of lymphoma:
Hodgkin lymphoma – People with this disease have abnormal lymphocytes that are called Reed-Sternberg cells. These cells usually form from B cells.
Non-Hodgkin lymphoma – This is a large group of cancers that start in lymphocytes. The cancers can grow quickly or slowly and can form from B cells or T cells.
Multiple Myeloma
Multiple myeloma is cancer that begins in plasma cells, another type of immune cell. The abnormal plasma cells, called myeloma cells, build up in the bone marrow and form tumors in bones all through the body. Multiple myeloma is also called plasma cell myeloma and Kahler disease.
Melanoma
Melanoma is cancer that begins in cells that become melanocytes, which are specialized cells that make melanin (the pigment that gives skin its color). Most melanomas form on the skin, but melanomas can also form in other pigmented tissues, such as the eye.
Brain and Spinal Cord Tumors
There are different types of brain and spinal cord tumors. These tumors are named based on the type of cell in which they formed and where the tumor first formed in the central nervous system. For example, an astrocytic tumor begins in star-shaped brain cells called astrocytes, which help keep nerve cells healthy. Brain tumors can be benign (not cancer) or malignant (cancer).
Other Types of Tumors
Germ Cell Tumors
Germ cell tumors are a type of tumor that begins in the cells that give rise to sperm or eggs. These tumors can occur almost anywhere in the body and can be either benign or malignant.
Neuroendocrine Tumors
Neuroendocrine tumors form from cells that release hormones into the blood in response to a signal from the nervous system. These tumors, which may make higher-than-normal amounts of hormones, can cause many different symptoms. Neuroendocrine tumors may be benign or malignant.
Carcinoid Tumors
Carcinoid tumors are a type of neuroendocrine tumor. They are slow-growing tumors that are usually found in the gastrointestinal system (most often in the rectum and small intestine). Carcinoid tumors may spread to the liver or other sites in the body, and they may secrete substances such as serotonin or prostaglandins, causing carcinoid syndrome.
Symptoms and Causes
Symptoms of cancer vary from person to person. They depend on what type of cancer you have and how advanced it is.
General cancer symptoms may include:
- Fatigue.
- Fever that occurs mostly at night.
- Loss of appetite.
- Night sweats.
- Persistent pain.
- Skin changes, particularly moles that change shape and size or new moles.
- Unexplained weight loss.
In some cases, cancer may cause organ-specific additional symptoms. This may include:
- Blood in your pee or stool.
- Change in the shape, color or size of skin mole.
- Coughing up blood.
- New lumps or bumps.
This isn’t an exhaustive list. And having these symptoms doesn’t necessarily mean you have cancer.
Cancer is a complicated disease. Different types cause different symptoms. It’s also possible to have cancer for years without knowing it. Other times, it can cause obvious symptoms that get worse very quickly.
A good rule of thumb is to let a healthcare provider know any time there’s a change in your body that lasts for more than two weeks.
What causes cancer?
Cancer is a genetic disorder. But that doesn’t necessarily mean it’s inherited. It happens when genes that manage cell activity mutate (change). They create abnormal cells that divide and multiply, eventually disrupting how your body works.
These cells create cancer clusters, or tumors. Cancerous cells may break away from tumors and travel to other areas of your body through your lymphatic system or bloodstream. (Healthcare providers call this metastasis.)
For example, a tumor in your breast may spread to your lungs, making it hard for you to breathe. In some types of blood cancer, your bone marrow makes abnormal blood cells that multiply uncontrollably. Eventually, the abnormal cells crowd out normal blood cells.
According to medical researchers, inherited genetic mutations (changes you can’t control) cause about 5% to 10% of all cancers. More often, cancer occurs as an acquired genetic mutation (change). That means it happens over the course of your life. Medical researchers have identified several risk factors that increase your chance of developing cancer.
Risk factors
There isn’t one single cause for cancer. Rather, certain things can increase your chance of developing it, like:
- Family history. If you have close biological family members (parents, siblings, grandparents) who have cancer, you have a higher risk of developing it.
- Smoking. Smoking tobacco or using e-cigarettes increases your chance of developing lung, esophageal, pancreatic and oral cancer.
- Environmental factors. Exposure to toxins in your environment, like asbestos, pesticides and radon, can eventually lead to cancer.
- Malnutrition. High-fat or high-sugar foods can increase your risk for many types of cancer. You’re also more vulnerable to disease if you don’t get enough physical activity.
- Hormone therapy. Women and people assigned female at birth (AFAB) taking hormone replacement therapy may have an increased risk for breast cancer and uterine cancer.
- Radiation exposure. Ultraviolet (UV) radiation from the sun significantly increases your risk of developing skin cancer. Over-exposure to radiation therapy can also be a risk factor.
Cancer Staging
Stage refers to the extent of your cancer, such as how large the tumor is and if it has spread. Knowing the stage of your cancer helps your doctor
- understand how serious your cancer is and your chances of survival
- plan the best treatment for you
- identify clinical trials that may be treatment options for you
A cancer is always referred to by the stage it was given at diagnosis, even if it gets worse or spreads. New information about how a cancer has changed over time is added to the original stage. So the stage doesn't change, even though the cancer might.
How Stage Is Determined
To learn the stage of your disease, your doctor may order x-rays, lab tests, and other tests or procedures. See the section on How Cancer Is Diagnosed to learn more about these tests.
Systems That Describe Stage
There are many staging systems. Some, such as the TNM staging system, are used for many types of cancer. Others are specific to a particular type of cancer. Most staging systems include information about
- where the tumor is located in the body
- the size of the tumor
- whether the cancer has spread to nearby lymph nodes
- whether the cancer has spread to a different part of the body

Most cancers have four stages. The specific stage is determined by a few different factors, including the tumor’s size and location.
Stage I-III (1-3) (early-stage or locally advanced) usually describes cancer when it has grown directly into surrounding tissue or has spread to nearby lymph nodes.
Stage IV (4) (or metastatic) means that cancer cells have spread to distant areas of your body through your bloodstream or lymphatic system.
The TNM Staging System
The TNM system is the most widely used cancer staging system. Most hospitals and medical centers use the TNM system as their main method for cancer reporting. You are likely to see your cancer described by this staging system in your pathology report unless there is a different staging system for your type of cancer. Examples of cancers with different staging systems include brain and spinal cord tumors and blood cancers.
In the TNM system
- The T refers to the size and extent of the main tumor. The main tumor is usually called the primary tumor.
- The N refers to the number of nearby lymph nodes that have cancer.
- The M refers to whether the cancer has metastasized. This means that the cancer has spread from the primary tumor to other parts of the body.
When your cancer is described by the TNM system, there will be numbers after each letter that give more details about the cancer—for example, T1N0MX or T3N1M0. The following explains what the letters and numbers mean.
Primary tumor (T)
- TX: Main tumor cannot be measured.
- T0: Main tumor cannot be found.
- T1, T2, T3, T4: Refers to the size and/or extent of the main tumor. The higher the number after the T, the larger the tumor or the more it has grown into nearby tissues. T's may be further divided to provide more detail, such as T3a and T3b.
- NX: Cancer in nearby lymph nodes cannot be measured.
- N0: There is no cancer in nearby lymph nodes.
- N1, N2, N3: Refers to the number and location of lymph nodes that contain cancer. The higher the number after the N, the more lymph nodes that contain cancer.
- MX: Metastasis cannot be measured.
- M0: Cancer has not spread to other parts of the body.
- M1: Cancer has spread to other parts of the body.
Another staging system that is used for all types of cancer groups cancer into one of five main categories. This staging system is more often used by cancer registries than by doctors.
- In situ—Abnormal cells are present but have not spread to nearby tissue.
- Localized—Cancer is limited to the place where it started, with no sign that it has spread.
- Regional—Cancer has spread to nearby lymph nodes, tissues, or organs.
- Distant—Cancer has spread to distant parts of the body.
- Unknown—There is not enough information to figure out the stage.
Ovarian Cancer
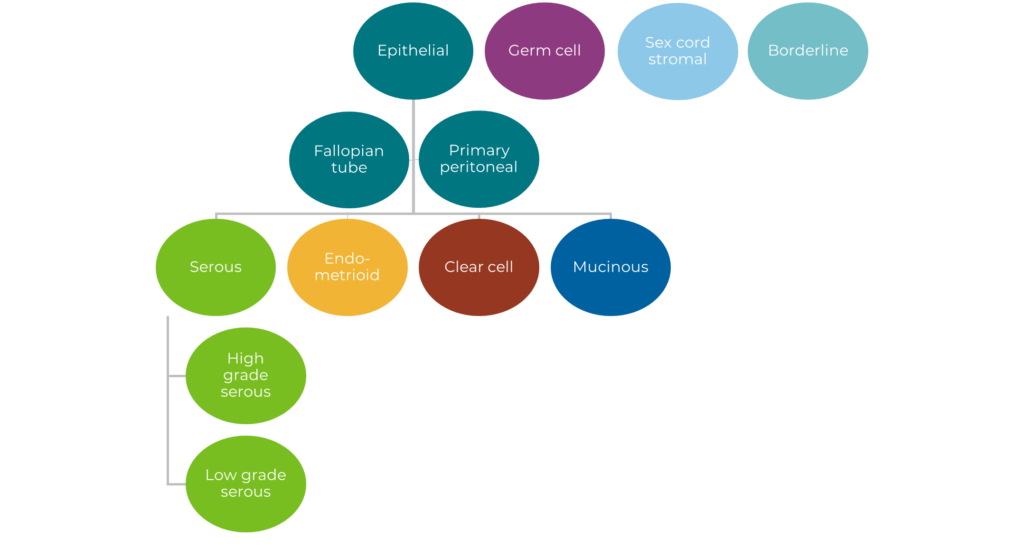
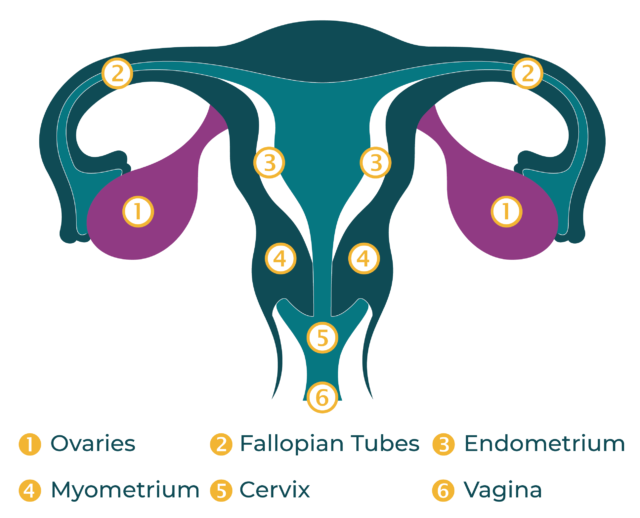
Ovarian cancer’ is not a singular diagnosis, rather it is an umbrella term for a multitude of different types of cancer that affect the ovaries, fallopian tubes, and the primary peritoneal cavity. It is estimated that there are more than 30 different types of ovarian cancer, and there is a very wide variation in incidence and outlook in terms of the different types.
Ovarian cancer is the most lethal of the female cancers for which there is no reliable screening test, and every person assigned female at birth is at risk. With delays in diagnoses due to this lack of screening and because symptoms are often confused with other, less severe, illness, most people are diagnosed once the cancer has already spread, making it more difficult to treat. While every woman is at risk, ovarian cancer is overlooked and underfunded.
Types of Ovarian Cancer
There are different types of ovarian cancer tumors, which are named after the type of cell they come from, the three main cell types that make up the ovary. They are:
Epithelial ovarian cancer
Comes from the surface of the ovary (the epithelium), and is the most common ovarian cancer. Fallopian tube cancer and primary peritoneal cancer are also included in this type of ovarian cancer.
Germ cell ovarian cancer
Comes from the reproductive cells of the ovaries. Germ cell ovarian cancer is rare.
Stromal cells ovarian cancer
Comes from connective tissue cell. Stromal cells ovarian cancer is also very rare.
Small cell carcinoma (SCCO) of the ovary
This is an extremely rare ovarian cancer and it is not certain whether the cells in SCCO are from ovarian epithelial cells, sex-cord stromal cells or germ cells.
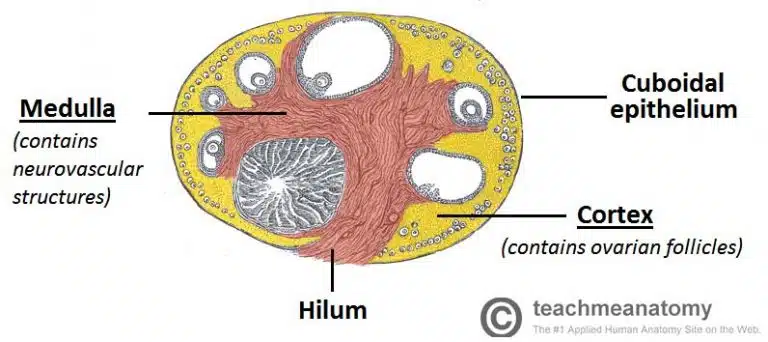
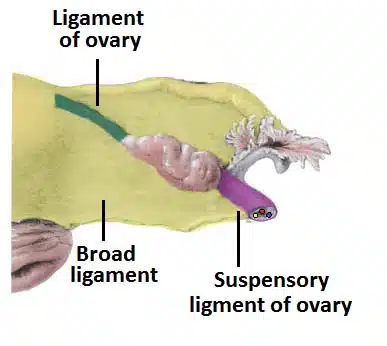
Anatomy of Ovaries
In both the males and females, the gonads develop within the mesonephric ridge and descend through the abdomen. However, unlike the testes, the ovaries stop in the pelvis.
The ovaries are paired, oval organs attached to the posterior surface of the broad ligament of the uterus by the mesovarium (a fold of peritoneum, continuous with the outer surface of the ovaries).
Neurovascular structures enter the hilum of the ovary via the mesovarium.
The main functions of the ovaries are:
- To produce oocytes (female gametes) in preparation for fertilizations.
- To produce the sex steroid hormones estrogen's and progesterone, in response to pituitary gonadotrophins (LH and FSH).
- Components of the Ovary
- The ovary has three main histological features:
- Surface – formed by simple cuboidal epithelium (known as germinal epithelium). Underlying this layer is a dense connective tissue capsule.
- Cortex – comprised of a connective tissue stroma and numerous ovarian follicles. Each follicle contains an oocyte, surrounded by a single layer of follicular cells.
- Medulla – formed by loose connective tissue and a rich neurovascular network, which enters via the hilum of the ovary.
Ovary Cancer facts
- A Pap test (cervical smear test) does not detect ovarian cancer
- Ovarian cancer is often diagnosed at a late stage
- Diagnosing ovarian cancer before it spreads makes it much more treatable
- Symptom awareness might lead to quicker diagnosis
- Common symptoms of ovarian cancer include:
a. Persistent bloating
b. Difficulty eating
c. Feeling full quickly
d. Pelvic/abdominal pain
e. Urinary symptoms
Causes
Ovarian cancer happens when there are changes (mutations) in the genetic material (DNA). Often, the exact cause of these genetic changes is unknown.
Most ovarian cancers are caused by genetic changes that happen during your lifetime. But sometimes these genetic changes are inherited, meaning that you are born with them. Ovarian cancer that is caused by inherited genetic changes is called hereditary ovarian cancer.
There are also certain genetic changes that can raise your risk of ovarian cancer, including changes called BRCA1 and BRCA2. These two changes also raise your risk of breast and other cancers.
Besides genetics, your lifestyle and the environment can affect your risk of ovarian cancer.
Who is more likely to develop ovarian cancer?
Certain people are more likely to develop ovarian cancer. They include those who:
- Have a family history of ovarian cancer in a mother, daughter, or sister
- Have inherited changes in the BRCA1 or BRCA2 genes.
- Have certain other genetic conditions, such as Lynch syndrome
- Have endometriosis
- Took hormone replacement therapy
- Are overweight or have obesity
- Are tall
- Are older, especially those who have gone through menopause
Common Signs and Symptoms
When ovarian cancer first develops, it might not cause any noticeable symptoms. When ovarian cancer symptoms happen, they're usually attributed to other, more common conditions.
Signs and symptoms of ovarian cancer may include:
- Abdominal bloating or swelling
- Quickly feeling full when eating
- Weight loss
- Discomfort in the pelvic area
- Fatigue
- Back pain
- Changes in bowel habits, such as constipation
- A frequent need to urinate
Reducing your risk of ovarian cancer
- While the following may reduce the risk of developing ovarian cancer, it is important to consider the risks, consequences, and potential side effects they may involve, and to remember that although these measures may lower your overall risk, there are currently no steps that you can take to 100% prevent ovarian cancer.
- Removal of ovaries and fallopian tubes
- Having your ovaries and fallopian tubes removed significantly reduces your chances of getting ovarian cancer. However, a rarer form of the disease can develop in the lining of the peritoneal cavity, so it does not remove all risk.
- Pregnancy and breast/natural feeding
- It is recognized that an increased number of ovulatory cycles raises the risk of ovarian cancer and conversely a decreased number of cycles (for example during pregnancy and lactation) reduces the risk.
- The contraceptive pill
- For every five years it is taken, hormonal contraception is known to reduce the risk of developing ovarian cancer by 20%.
Ovarian Cancer Key stats
According to Globocan’s 2022 projections, by 2050, the number of women around the world diagnosed with ovarian cancer will rise over 55% to 503,448. The number of women dying from ovarian cancer each year is projected to increase to 350,956 an increase of almost 70% from 2022.
Five-year ovarian cancer survival rates vary between countries. For example, in more developed countries, current rates range from 36% to 46%. However, in some countries the figure is much lower. Overall, survival rates fall well below that for other cancers, like breast cancer, where five-year survival rates in many countries are close to 90%.
Ovarian cancer is a global concern and much more needs to be done to tackle this disease on all fronts. Based these 2022 Globocan mortality rates, if nothing changes, it is estimated that over eight million women will die from ovarian cancer worldwide. The majority of lives lost will be from low- and middle-income countries where 70% of those diagnosed live.

Diagnosis and Tests
If you have a symptom or a screening test result that suggests cancer, your doctor will find out whether it is due to cancer or some other cause. There is no single test that can diagnose cancer. So your doctor may start by asking about your personal and family medical history and doing a physical exam. They may order lab tests, imaging tests (scans), or other tests or procedures. You may also need a biopsy, which is often the only way to tell for sure if you have cancer.
Making sense of test results
Results from lab tests, imaging, and biopsies are often posted in your patient portal before your doctor can discuss them with you. It is normal to feel anxious and want to know right away what the results are and what they mean. But your doctor is the best person to explain the results from all your tests and what they mean for you.
Lab tests used to diagnose cancer
High or low levels of certain substances in your body can be a sign of cancer. So lab tests of your blood, urine, and other body fluids that measure these substances can help doctors make a diagnosis. However, abnormal lab results are not a sure sign of cancer. Lab test results are used along with the results of other tests, such as biopsies and imaging, to help diagnose and learn more about a person’s cancer.
It is important to keep in mind that lab results for healthy people can vary from person to person. Reasons for these differences include age, sex, race, medical history, and general health. In fact, your own results can vary from day to day. Because normal results can bounce around a bit, they are often reported in a range, with lower and upper limits. These ranges are based on test results from large numbers of people who have been tested in the past.
For many tests, it is possible to have normal results even if you have cancer. And it is possible to have test results outside the normal range even if you are healthy.
Some common types of lab tests used to help diagnose cancer are listed below.
Blood chemistry test
What it does: A blood chemistry test measures the amounts of certain substances that are released into the blood by the organs and tissues of the body. These substances include metabolites, electrolytes, fats, sugars, and proteins, including enzymes.
What it tells us: Blood chemistry tests give important information about how well your kidneys, liver, and other organs are working. High or low levels of some substances in the blood can be a sign of disease or treatment side effects.
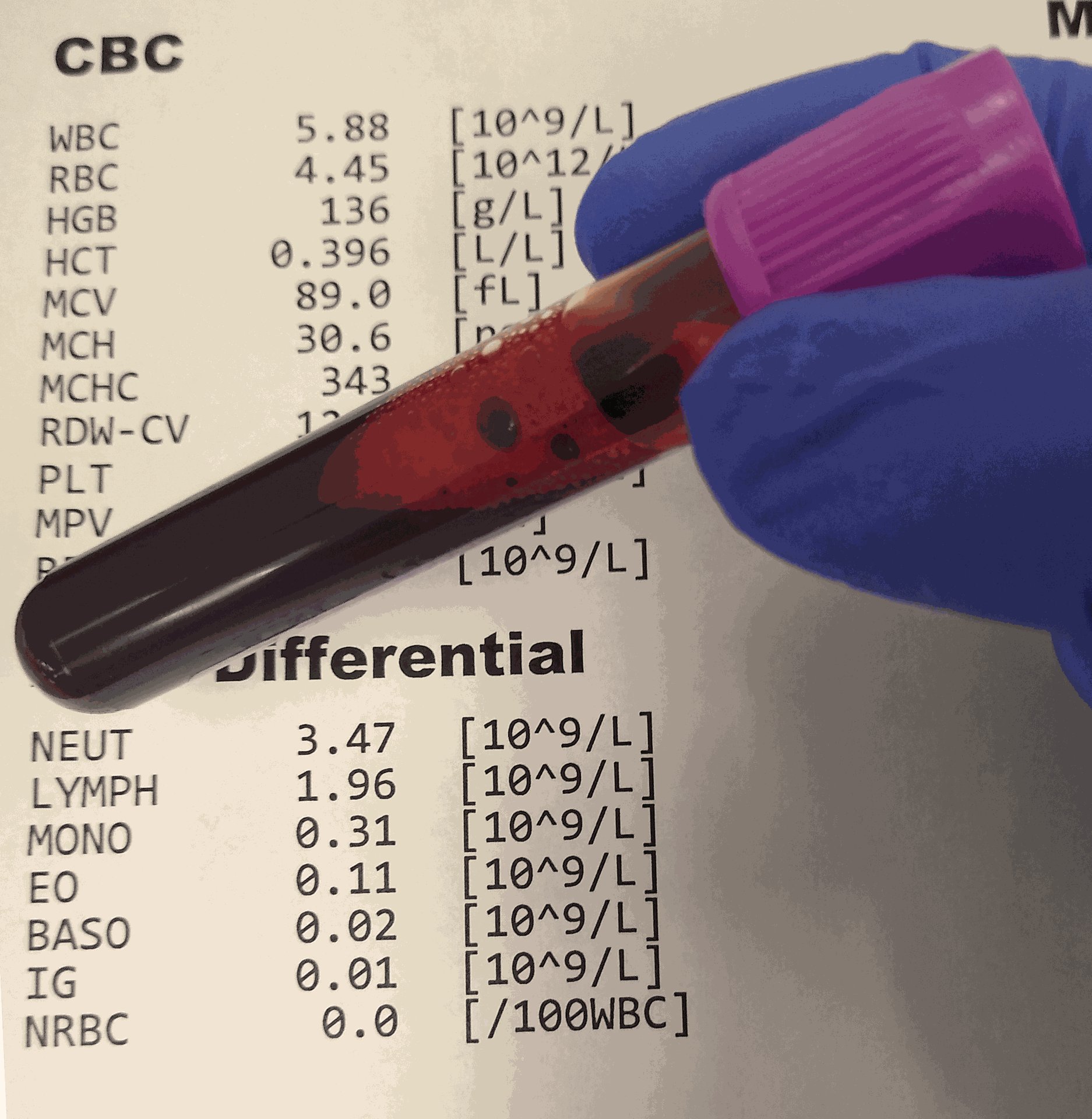
Complete blood count (CBC)
What it does: The CBC measures the number of red blood cells, white blood cells, and platelets in your blood. It also measures the amount of hemoglobin (the protein that carries oxygen) in your blood, the amount of your blood that is made up of red blood cells (hematocrit), the size of your red blood cells, and the amount of hemoglobin in your red blood cells.
How it is used: The CBC is often part of a routine health check-up. It can help diagnose some cancers, especially leukemias. It is also used to monitor your health during and after treatment.
Cytogenetic analysis
What it does: Cytogenetic analysis looks for changes in chromosomes in samples of tissue, blood, bone marrow, or amniotic fluid. Chromosome changes may include broken, missing, rearranged, or extra chromosomes. Changes in certain chromosomes may be a sign of a genetic condition or some types of cancer.
How it is used: Cytogenetic analysis may be used to help diagnose cancer, plan treatment, or find out how well treatment is working.
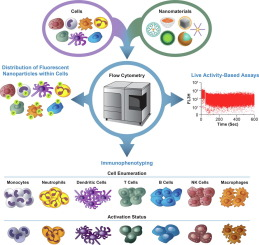
Immunophenotyping
What it does: Immunophenotyping uses antibodies to identify cells based on the types of antigens or markers on the surface of the cells. It is most often done on blood or bone marrow samples. But it may also be done on other body fluids or tissue samples.
How it is used: Immunophenotyping helps diagnose, stage, and monitor blood cancers and other blood disorders, such as leukemias, lymphomas, myelodysplastic syndromes, and myeloproliferative disorders.
Liquid biopsy
What it does: Liquid biopsy is a test done on a sample of blood to look for cancer cells or pieces of DNA from tumor cells that are sometimes released into the blood.
How it is used: A liquid biopsy may help find cancer at an early stage. It may also be used to help plan treatment or to find out how well treatment is working or if cancer has come back.
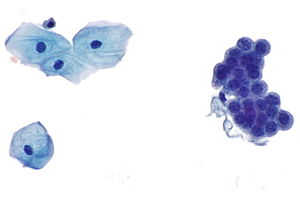
Sputum cytology
What it does: Sputum cytology looks for abnormal cells in sputum, which is mucus and other matter brought up from the lungs by coughing.
How it is used: Sputum cytology can help diagnose lung cancer.
Tumor marker tests
What they do: Tests for tumor markers measure substances that are produced by cancer cells or other cells of the body in response to cancer. Most tumor markers are made by both normal cells and cancer cells. But they are produced at much higher levels by cancer cells.
How they are used: Tumor markers can be used to help diagnose cancer, decide on treatment, measure how well treatment worked, and watch for signs that the cancer has returned.
Urinalysis
What it does: Urinalysis describes the color of urine and measures its contents, such as sugar, protein, red blood cells, and white blood cells.
How it is used: Urinalysis can help diagnose kidney cancer, bladder cancer, and rarer urothelial cancers.
Urine cytology
What it does: Urine cytology finds disease by looking for abnormal cells shed from the urinary tract into the urine.
How it is used: Urine cytology helps diagnose kidney cancer, bladder cancer, and rarer urothelial cancers. After cancer treatment, it is used to watch for signs that cancer has returned.
Imaging tests used in cancer
Imaging tests create pictures of areas inside your body that help the doctor see whether a tumor is present. These pictures can be made in several ways.
CT scan
A CT scan uses an x-ray machine linked to a computer to take a series of pictures of your organs from different angles. These pictures are used to create detailed 3-D images of the inside of your body.
Sometimes, you may receive a dye or other contrast material before you have the scan. You might swallow the dye, or it may be given by a needle into a vein. Contrast material helps make the pictures easier to read by highlighting certain areas in the body.
During the CT scan, you will lie still on a table that slides into a donut-shaped scanner. The CT machine moves around you, taking pictures.
MRI
An MRI uses a powerful magnet and radio waves to take pictures of your body in slices. These slices are combined to create detailed images of the inside of your body, which can show places where there may be tumors.
When you have an MRI, you lie still on a table that is pushed into a long chamber that surrounds part or all of your body. The MRI machine makes loud thumping noises and rhythmic beats.
Sometimes, you might have a special dye injected into your vein before or during your MRI exam. This dye, called a contrast agent, can make tumors show up brighter in the pictures.
Nuclear scan
A nuclear scan uses radioactive material to take pictures of the inside of the body. This type of scan may also be called a radionuclide scan.
Before this scan, you receive an injection of a small amount of radioactive material, which is sometimes called a tracer. It flows through your bloodstream and collects in certain bones or organs.
During the scan, you lie still on a table while a machine called a scanner detects and measures the radioactivity in your body, creating pictures of bones or organs on a computer screen or on film.
After the scan, the radioactive material in your body will lose its radioactivity over time. It may also leave your body through your urine or stool.
Bone scan
Bone scans are a type of nuclear scan that check for abnormal areas or damage in the bones. They may be used to diagnose bone cancer or find out whether cancer has spread to the bones from elsewhere in the body (called metastatic bone tumors).
Before this test, a very small amount of radioactive material is injected into your vein. As it travels through the blood, the material collects in abnormal areas in the bone. Areas where the material collects show up on pictures taken by a special scanner. These areas are called “hot spots.”
PET scan
A PET scan is a type of nuclear scan that makes detailed 3-D pictures of areas inside your body where glucose is taken up. Because cancer cells often take up more glucose than healthy cells, the pictures can be used to find cancer in the body.
Before the scan, you receive an injection of a tracer called radioactive glucose. During the scan, you will lie still on a table that moves back and forth through a scanner.
Ultrasound
An ultrasound exam uses high-energy sound waves that people cannot hear. The sound waves echo off tissues inside your body. A computer uses these echoes to create pictures of areas inside your body. This picture is called a sonogram.
During an ultrasound exam, you will lie on a table while a technologist slowly moves a device called a transducer, which makes the high-energy sound waves, on the skin over the part of the body that is being examined. The transducer is covered with a warm gel that helps it glide over the skin.
X-rays
X-rays use low doses of radiation to create pictures inside your body. An x-ray technologist will put you in position and direct the x-ray beam to the correct part of your body. While the images are taken, you will need to stay very still and may need to hold your breath for a second or two.
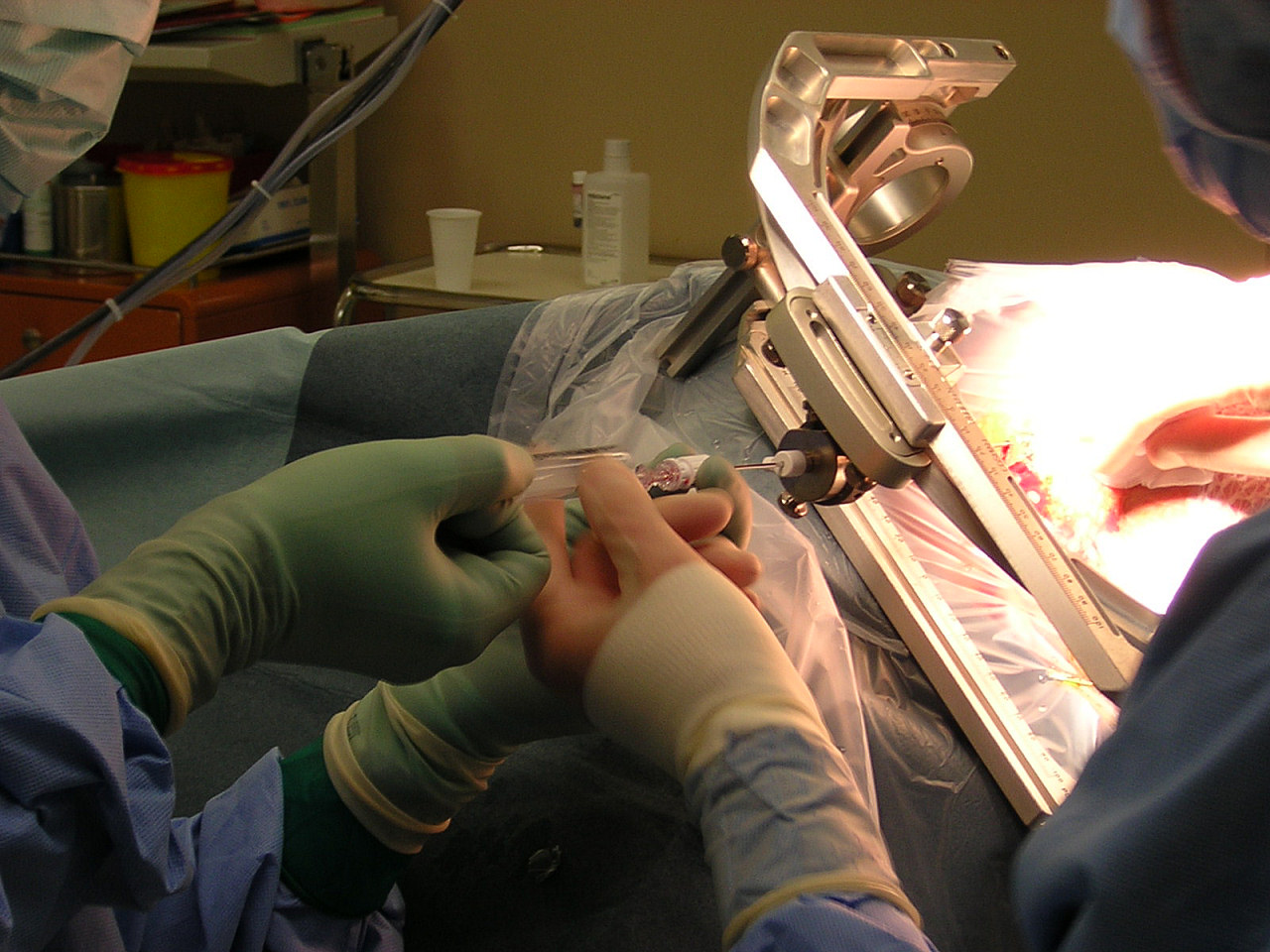
Biopsy
In most cases, doctors need to do a biopsy to be certain that you have cancer. A biopsy is a procedure in which the doctor removes a sample of abnormal tissue. A pathologist looks at the tissue under a microscope and runs other tests on the cells in the sample. The pathologist describes the findings in a pathology report, which contains details about your diagnosis. The information in your pathology reports can also help show what treatment options might work for you.
The biopsy sample may be obtained in several ways.
With a needle: The doctor uses a needle to withdraw tissue or fluid. This method is used for bone marrow aspirations, spinal taps, and some breast, prostate, and liver biopsies.
With endoscopy: The doctor inserts a thin, lighted tube called an endoscope into a natural body opening, such as the mouth or anus. The doctor can remove some or all of the abnormal tissue through the endoscope.
Examples of endoscopy exams include:
- Colonoscopy, which is an exam of the colon and rectum. In this type of exam, an endoscope goes through the anus.
- Bronchoscopy, which is an exam of the trachea, bronchi, and lungs. In this type of exam, an endoscope goes through the mouth or nose and down the throat.
With surgery: A surgeon removes an area of abnormal cells during an operation. Surgery may be excisional or incisional.
In an excisional biopsy, the surgeon removes the entire area of abnormal cells. Often some of the normal tissue around these cells is also removed.
In an incisional biopsy, the surgeon removes just part of the abnormal area.
Some biopsies may require a sedative or anesthesia.
Sedatives are medicine that helps you relax and stay very still or sleep during a biopsy.
Anesthesia keeps you from feeling pain. It refers to drugs or other substances that cause you to lose feeling or awareness. There are three types of anesthesia.
- local anesthesia, which causes loss of feeling in one small area of the body
- regional anesthesia, which causes loss of feeling in a part of the body, such as an arm or leg
- general anesthesia, which causes loss of feeling and a complete loss of awareness that seems like a very deep sleep
What happens if tests show you have cancer
If the biopsy and other tests show that you have cancer, you may have more tests to help your doctor plan treatment. For instance, your doctor may do other tests to figure out if the cancer has spread and how far. This information is important for knowing the stage of your cancer. For some cancers, other pathology studies are done to find out the grade of the tumor. Or tumor markers are studied to find out the risk group that you fall into. This information is important for deciding on the best treatment. Your tumor may also be tested further for other tumor markers or biomarkers.
Management and Treatment
How is cancer treated?
Healthcare providers may use several different treatments, sometimes combining treatments based on your situation. Common cancer treatments include:
- Surgery: Can remove cancerous tumors that haven’t spread.
- Chemotherapy: Destroys cancer cells with powerful drugs in pill form or intravenously (through a needle into a vein).
- Radiation therapy: Kills cancer cells with high dosages of radiation.
- Immunotherapy: Engages your immune system to fight the disease.
- Targeted therapy: Targets the genetic mutations (changes) that turn healthy cells into cancer cells.
- Hormone therapy: Blocks cancer-causing hormones. For example, people assigned male at birth who have prostate cancer might receive hormones to lower testosterone, which can contribute to prostate cancer.
- Bone marrow transplant: Replaces damaged blood stem cells with healthy ones.
Cancer treatments can cause several side effects. These side effects vary depending on which treatment you have and how your body tolerates it. If you develop side effects during your cancer treatment, let your healthcare provider know. They may be able to give you recommendations or medications that can help.
Prevention
Can cancer be prevented?
You can’t always prevent cancer, especially when unavoidable risk factors cause it. But there are things you can do to lower your risk:
- If you smoke or use tobacco, try to stop. Ask a healthcare provider about smoking cessation programs that can help you quit tobacco.
- Follow a nutrition plan that’s healthy for you.
- Include physical activity in your daily routine.
- Avoid environmental toxins like asbestos and pesticides.
- Protect yourself against sun damage.
- Have regular cancer screenings.
Outlook/Prognosis
What is the outlook for cancer?
You are unique, and so is your prognosis. Your healthcare providers will base your outlook on factors like:
- Your overall health.
- The type of cancer you have.
- The stage of your cancer.
- How you respond to treatment.
While there’s no single cure for cancer, some cancers respond well to treatment. Many people notice a reduction in their signs and symptoms. When this happens, healthcare providers call it remission. Partial remission is when you have fewer signs and symptoms. Complete remission is when you no longer experience symptoms at all.
Different cancers require different treatments, so outcomes vary. In general, people who receive their diagnosis and begin treatment before cancer spreads have a more positive outlook. But even if your cancer has spread beyond where it started, treatment can slow its growth, ease your symptoms, help you live longer and improve your quality of life.
What are cancer survival rates?
Survival rates are estimates based on the experiences of large groups of people with different kinds of cancer. Like prognoses, survival rates vary based on cancer type, stage and treatment.
It’s important to remember that survival rates are only estimates. They can’t tell you how long you’ll live or how your body will respond to certain treatments. Your healthcare provider can tell you more about survival rates and what they mean for you.
FAQ(Frequently Asked Questions)
How do I recognize cancer before it starts to cause serious health problems?
Some cancers cause early symptoms, but others do not exhibit symptoms until they are more advanced. Many of these symptoms are often from causes unrelated to cancer.
The best way to identify cancer early is to report any unusual, persistent symptoms to a doctor so they can offer advice about any further testing that may be needed.
Can people with cancer live a long life?
Each individual’s outlook varies depending on the type of cancer they have and other factors, such as their overall health and whether the disease has spread.
However, the ACS indicates that the overall cancer death rate has declined by 33%.
How long can someone live with cancer without knowing?
Some types of cancer do not cause symptoms in the early stages. Therefore, a person may not know they are living with the disease until it reaches more advanced stages.
For example, research indicates that carcinoid tumors may not present with any symptoms for years.
References
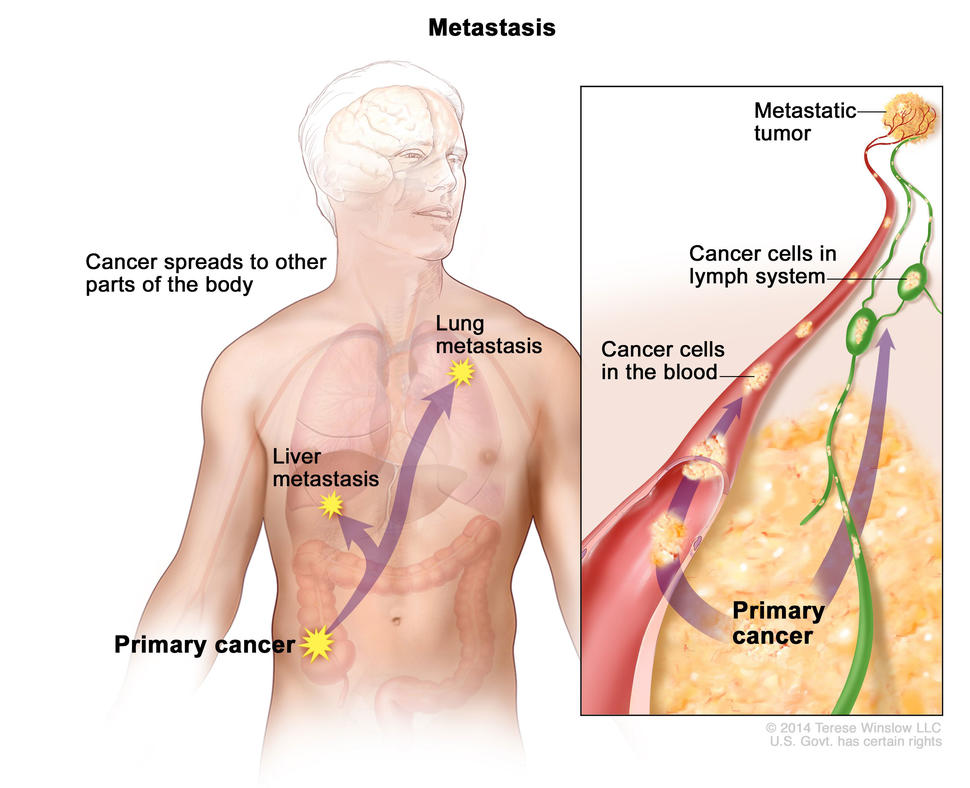 In metastasis, cancer cells break away from where they first formed and form new tumors in other parts of the body.
In metastasis, cancer cells break away from where they first formed and form new tumors in other parts of the body.
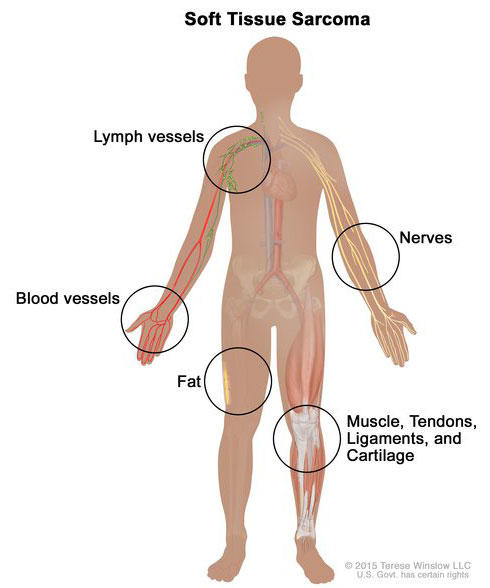 Soft tissue sarcoma forms in soft tissues of the body, including muscle, tendons, fat, blood vessels, lymph vessels, nerves, and tissue around joints.
Soft tissue sarcoma forms in soft tissues of the body, including muscle, tendons, fat, blood vessels, lymph vessels, nerves, and tissue around joints.
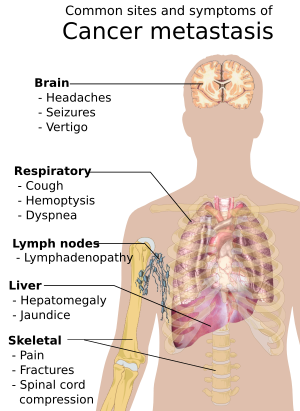 Symptoms of metastasis cancer depend on the location of the tumor.
Symptoms of metastasis cancer depend on the location of the tumor.